A physician-led medical approach designed to address the underlying drivers of metabolic and whole-body health.
Weight gain often reflects changes in metabolism, hormones, and physiology, not a lack of effort.
Serving TN, IN, KY, MO & AL — expanding soon
At ReNouvele™, care is physician-led from the beginning. Each patient completes a medical intake and clinical review to help identify factors that may be contributing to changes in weight and overall health, and to determine what approach is medically appropriate and safe.
Every intake is reviewed by a licensed, board-certified physician. Decisions are based on medical history, clinical judgment, and evidence-based care, not algorithms.

All patients are reviewed for safety and eligibility. Submitting an intake does not guarantee treatment. Care decisions are made medically, not commercially.

Treatment plans are individualized. Care may include nutrition guidance, lifestyle strategies, and medication when clinically appropriate.

Care does not end after the first visit. Follow-up and continuity of care are part of a responsible medical approach.

Care is delivered through secure, state-compliant telehealth platforms with proper documentation and follow-up.
ReNouvele™ is built around medical decision-making rather than trends or one-size-fits-all programs. Care focuses on understanding factors that may contribute to changes in weight and metabolic health, and determining what approach, if any, is medically appropriate.

Thorough health assessment to guide treatment decisions.

Care led by a licensed physician for personalized plans.

Identifying hormonal, metabolic, and lifestyle factors.

Continued monitoring and support for lasting results.
Founder ReNouvele™
Lasting health isn’t built on quick fixes. It starts with listening to the body, understanding physiology, and creating care that is safe, realistic, and sustainable.
Dr. Elizabeth Rodriguez is a board-certified physician known for combining clinical rigor with genuine compassion. She believes high-quality care begins with listening, thoughtful evaluation, and medical decision-making grounded in science rather than trends.
She is board-certified in Family Medicine and Obesity Medicine and completed advanced fellowship training in obesity medicine. Before becoming a physician, Dr. Rodriguez practiced as a registered nurse, providing hands-on patient care across diverse clinical settings. That foundation continues to shape her approach today, with an emphasis on whole-person health, safety, and long-term outcomes.
At ReNouvele™, Dr. Rodriguez provides physician-led care focused on restoring metabolic and whole-body health. Each patient receives an individualized evaluation, clear education, and treatment recommendations based on medical eligibility, clinical judgment, and sustainability over time. Weight management may be one component of care, but the broader goal is improved health, function, and confidence from the inside out.
Patients often describe Dr. Rodriguez as attentive, approachable, and deeply invested in their well-being. Her mission is to help patients feel informed, supported, and empowered in their health today and in the years ahead.

ReNouvele™ offers physician-led medical care focused on metabolic health and weight-related concerns through secure virtual visits. Each patient receives individualized evaluation and guidance based on medical history, safety considerations, and long-term health goals.
 Custom Plans
Custom Plans
 Certified Physician
Certified Physician
 Personalized Protocols
Personalized Protocols
 Performance Monitoring
Performance Monitoring
Step 01:
Patients complete a secure medical intake that includes health history, current medications, and relevant risk factors.
This information allows the physician to understand what may be contributing to weight gain and determine whether care may be appropriate.
Step 02:
A licensed clinician reviews the intake information to assess medical eligibility and clinical risk.
Submitting an intake does not guarantee treatment. No medications are prescribed without physician review.
Step 03:
When medically appropriate, patients may receive a personalized care plan based on clinical judgment, safety considerations, and long-term health goals.
Care may include nutrition guidance, lifestyle strategies, and medication management with ongoing medical oversight.
Support your health with individualized, physician-led medical care focused on metabolism and whole-body function. Care begins with a medical intake and clinical review to understand what may be contributing to changes in weight and health over time.
Custom oral medication kits,
taken daily and starting at
$129/mo

Weight changes often reflect shifts inside the body over time. This section provides educational information about common medical and physiologic factors that can influence metabolism, body composition, and long-term health.
This information is for education only and does not replace a medical evaluation.
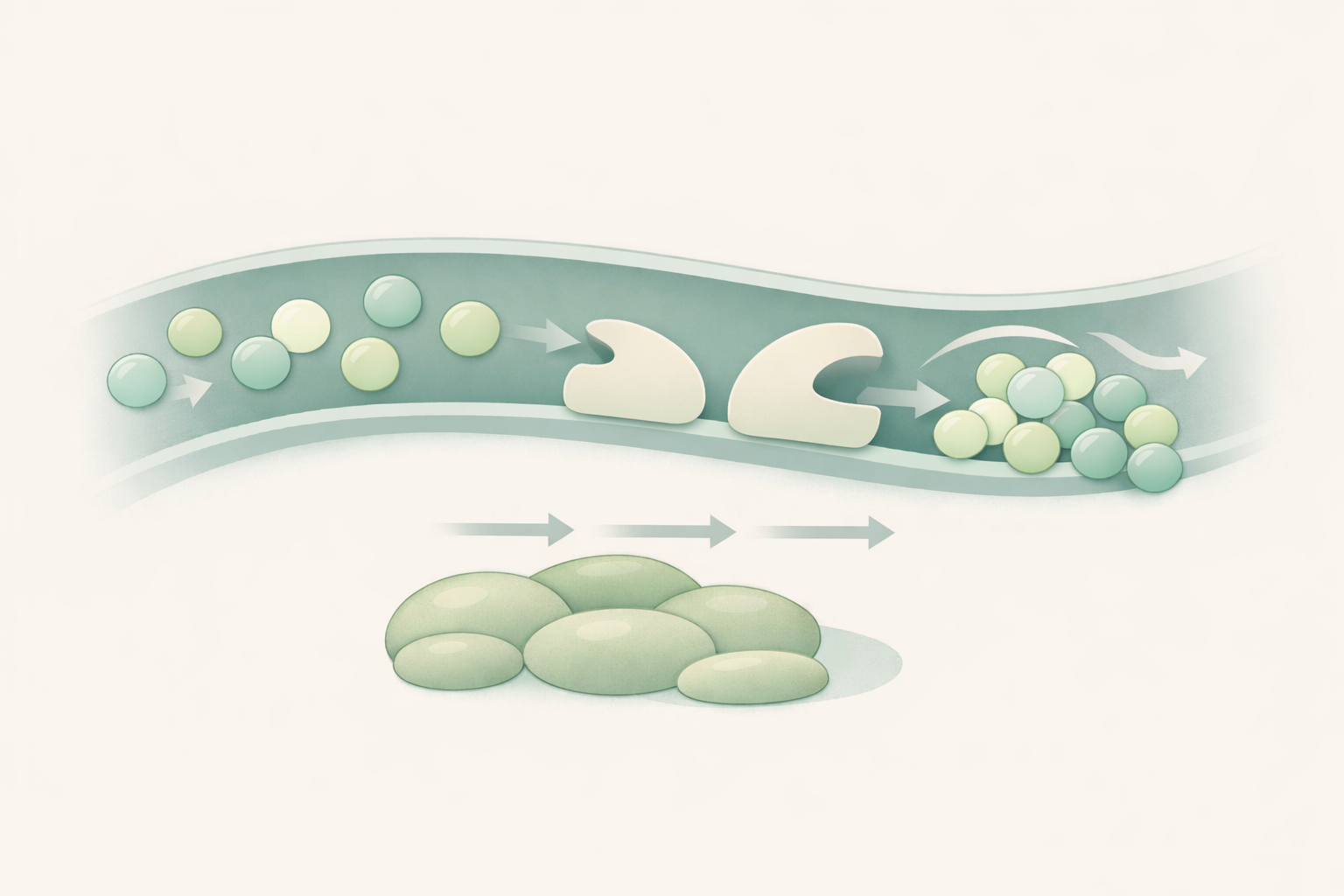
When the body does not respond effectively to insulin, blood sugar regulation can change. This may influence how energy is stored and used over time and can be associated with changes in weight and metabolic health.

Hormones play a key role in regulating appetite, energy use, and metabolic function. Changes related to age, stress, or underlying health conditions can influence weight patterns and overall metabolic balance.

Long-term inflammation can affect how the body processes and utilizes energy. Over time, this may contribute to metabolic changes, fatigue, and challenges related to maintaining overall metabolic health.
After repeated dieting or weight cycling, the body may adapt by conserving energy. This physiologic response can affect metabolic efficiency and influence how the body responds to future changes in nutrition or activity.
Fat accumulation in the liver is associated with insulin resistance and broader metabolic changes. This condition may develop gradually and is often evaluated as part of a comprehensive metabolic assessment.
Sleep quality and stress hormones influence appetite regulation, blood sugar balance, and energy storage. Disruptions in these systems over time can affect metabolic health and overall physiologic function.
Dedicated to providing expert healthcare advanced technology, experienced professionals, and personalized treatments to ensure your well-being and a healthier future.
"ReNouvele™ feels different from other programs. Everything was explained clearly, and I never felt pressured into decisions.”!"
This is medical care.
ReNouvele provides physician-led medical evaluation and treatment focused on metabolic and whole-body health, including weight-related concerns. Care is based on clinical assessment, medical history, and safety considerations—not coaching programs or motivational guidance.
No.
Completing the intake does not guarantee treatment. All submissions are reviewed for medical safety and eligibility. Treatment is provided only when clinically appropriate.
Physician-led care means all medical decisions are made by a licensed, board-certified physician.
Your intake, eligibility, and treatment plan are medically reviewed to determine what approach is appropriate for your health and safety.
Some individuals may not be eligible based on medical history, current conditions, medications, pregnancy or breastfeeding status, or other safety considerations.
Eligibility is determined through medical review. If care is not appropriate, treatment will not be provided.
This care may be appropriate for adults who have experienced changes in weight, metabolism, or overall health related to hormonal, metabolic, or long-term physiologic factors.
Patients seeking medically supervised care focused on metabolic and whole-body health rather than coaching or one-size-fits-all programs may benefit from this approach.
No.
Medication is not prescribed to every patient. Treatment recommendations are individualized and based on medical need, safety, and clinical judgment.
GLP-1 medications may be prescribed when medically appropriate.
Not all patients are candidates. Eligibility is determined through medical evaluation, clinical judgment, and safety considerations.
Treatment plans may include medical evaluation, lifestyle and nutrition guidance, and medication management when clinically indicated.
Care is individualized and may address metabolic health, weight-related concerns, and other factors that influence overall health and long-term wellbeing.
ReNouvele is built around a physician-led approach focused on supporting how the body functions over time.
Care emphasizes metabolic health, hormonal balance, and other physiologic factors that influence energy, body composition, and overall wellbeing. Weight-related concerns may be one part of care, but the broader goal is long-term health, resilience, and overall wellness.
Care at ReNouvele is guided by medical appropriateness and individual health needs.
As the practice evolves, services may expand to support broader aspects of health and wellbeing. Any care offered is evaluated through a medical lens and provided only when clinically appropriate.
Care does not end after the initial visit.
When treatment is provided, follow up and ongoing medical oversight are part of responsible care. The frequency and structure of follow up depend on the treatment plan and clinical needs.
Care is delivered through secure, state compliant telehealth platforms.
Patients complete a medical intake and receive care remotely when legally permitted in their state. Documentation and follow up are part of the medical process.
ReNouvele does not bill insurance directly.
Patients may choose to use eligible health savings or flexible spending accounts depending on their plan. Medication coverage varies by insurance provider.
ReNouvele currently provides care to patients located in Indiana, Tennessee, Alabama, Kentucky, and Missouri.
Care is delivered via telehealth where legally permitted and based on physician licensure.
Additional states may be added as licensure and regulatory requirements are met.
Schedule your healthcare visit in just a few steps. Fill out the form below and our team will confirm your appointment immediately.
Warning
Drugs like this one have raised the chance of suicidal thoughts or actions in children and young adults. The risk may be greater in people who have had these thoughts or actions in the past. All people who take this drug need to be watched closely. Call the doctor right away if signs like depression, nervousness, restlessness, grouchiness, panic attacks, or changes in mood or actions are new or worse. Call the doctor right away if any thoughts or actions of suicide occur.
What is this drug used for?
What do I need to tell my doctor BEFORE I take this drug?
This is not a list of all drugs or health problems that interact with this drug.
Tell your doctor and pharmacist about all of your drugs (prescription or OTC, natural products, vitamins) and health problems. You must check to make sure that it is safe for you to take this drug with all of your drugs and health problems. Do not start, stop, or change the dose of any drug without checking with your doctor.
What are some things I need to know or do while I take this drug?
For all patients taking this drug:
You will need to talk about the benefits and risks to you and the baby.
If you smoke:
What are some side effects that I need to call my doctor about right away? WARNING/CAUTION:
Even though it may be rare, some people may have very bad and sometimes deadly side effects when taking a drug. Tell your doctor or get medical help right away if you have any of the following signs or symptoms that may be related to a very bad side effect:
What are some other side effects of this drug?
All drugs may cause side effects. However , many people have no side effects or only have minor side effects. Call your doctor or get medical help if any of these side effects or any other side effects bother you or do not go away:
All products:
Extended-release tablets:
How is this drug best taken?
Use this drug as ordered by your doctor. Read all information given to you. Follow all instructions closely.
For all uses of this drug:
What do I do if I miss a dose?
How do I store and/or throw out this drug?
General drug facts
Metformin is approved by the FDA as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus. Healthcare providers have the discretion to prescribe a medication for other uses as part of the practice of medicine.
Important Safety Information
Metformin is a prescription medicine that is FDA approved to treat Type 2 diabetes mellitus when hyperglycemia cannot be managed with diet and exercise alone.
When prescribed off-label Metformin may help some adults with overweight or obesity lose weight and keep the weight off.
What is the most important information I should know about Metformin tablets?
Serious side effects can happen in people taking Metformin tablets, including:
Lactic Acidosis. Metformin, the medicine in Metformin tablets, can cause a rare, but serious, side effect called lactic acidosis (a build-up of lactic acid in the blood) that can cause death. Lactic acidosis is a medical emergency and must be treated in a hospital.
Stop taking Metformin tablets and call your healthcare provider right away if you get any of the following symptoms of lactic acidosis:
Feel very weak and tired
Have unusual (not normal) muscle pain
Have trouble breathing
Have unusual sleepiness or sleep longer than usual
Have unexplained stomach or intestinal problems with nausea and vomiting, or diarrhea
Feel cold, especially in your arms and legs
Feel dizzy or lightheaded
Have a slow or irregular heartbeat
You have a higher chance of getting lactic acidosis if you:
Have kidney problems. People whose kidneys are not working properly should not take Metformin tablets.
Have liver problems.
Have congestive heart failure that requires treatment with medicines.
Drink a lot of alcohol (very often or short-term “binge” drinking).
Get dehydrated (lose a large amount of body fluids). This can happen if you are sick with a fever, vomiting, or diarrhea. Dehydration can also happen when you sweat a lot with activity or exercise and do not drink enough fluids.
Have certain x-ray tests with injectable dyes or contrast agents.
Have surgery.
Have a heart attack, severe infection, or stroke.
Are 80 years of age or older and have not had your kidney function tested.
Do not take Metformin tablets if you:
Have kidney problems
Have an abnormal creatinine level (not to exceed 500mg daily)
Are allergic to the metformin in Metformin tablets or any of the ingredients in Metformin tablets. See the medication guide for the full list of ingredients.
Are going to get an injection of dye or contrast agents for an x-ray procedure or if you are going to have surgery and not able to eat or drink much. In these situations, Metformin tablets will need to be stopped for a short time. Talk to your healthcare provider about when you should stop Metformin tablets and when you should start Metformin tablets again.
What should I tell my healthcare provider before taking Metformin tablets?
Before taking Metformin tablets, tell your healthcare provider if you:
Have type 1 diabetes. Metformin tablets should not be used to treat people with type 1 diabetes.
Have a history or risk for diabetic ketoacidosis (high levels of certain acids, known as ketones, in the blood or urine). Metformin tablets should not be used for the treatment of diabetic ketoacidosis.
Have kidney problems.
Have an abnormal creatinine level
Have liver problems.
Have heart problems, including congestive heart failure.
Are older than 80 years. If you are over 80 years old you should not take Metformin tablets unless your kidneys have been checked and they are normal.
Drink alcohol very often, or drink a lot of alcohol in short-term “binge” drinking.
Are taking insulin.
Have any other medical conditions.
Are pregnant or plan to become pregnant. It is not known if metformin will harm your unborn baby. If you are pregnant, talk with your healthcare provider about the best way to control your blood sugar while you are pregnant.
Are breast-feeding or plan to breast-feed. It is not known if metformin passes into your breast milk. Talk with your healthcare provider about the best way to feed your baby while you take Metformin tablets.
Tell your healthcare provider about all the medicines you take, including prescription and nonprescription medicines, vitamins, and herbal supplements. Know the medicines you take. Keep a list of them to show your healthcare provider and pharmacist when you get a new medicine.
Metformin tablets may affect the way other medicines work, and other medicines may affect how Metformin tablets work.
Common side effects of Metformin tablets include diarrhea, nausea, and upset stomach. These side effects generally go away after you take the medicine for a while. Taking your medicine with meals can help reduce these side effects. Tell your healthcare provider if the side effects bother you a lot, last for more than a few weeks, come back after they’ve gone away, or start later in therapy. You may need a lower dose or need to stop taking the medicine for a short period or for good.
About 3 out of every 100 people who take Metformin tablets have an unpleasant metallic taste when they start taking the medicine. It lasts for a short time.
Metformin tablets rarely cause hypoglycemia (low blood sugar) by themselves. However, hypoglycemia can happen if you do not eat enough, if you drink alcohol, or if you take other medicines to lower blood sugar.
You are encouraged to report negative side effects of prescription drugs to the FDA. Visit www.fda.gov/medwatch or call 1-800-FDA-1088.
The above health information is provided for educational purposes only and is not intended to replace discussions with a healthcare provider. All decisions regarding patient care must be made with a healthcare provider, considering the unique characteristics of the patient. The product information provided is intended only for residents of the United States. The products discussed herein may have different product labeling in different countries.
Topiramate is FDA approved
to treat certain types of seizures (partial-onset seizures and primary generalized tonic-clonic seizures) in adults and children 2 years and older.
with other medicines to treat certain types of seizures (partial-onset seizures, primary generalized tonic-clonic seizures, and seizures associated with Lennox-Gastaut syndrome) in adults and children 2 years and older.
to prevent migraine headaches in adults and adolescents 12 years and older.
Topiramate is prescribed off-label and may help some adults with overweight and obesity lose weight and keep the weight off.
Important Safety Information
What is the most important information I should know about Topiramate?
Topiramate may cause eye problems. Serious eye problems include:
Any sudden decrease in vision with or without eye pain and redness.
A blockage of fluid in the eye causing increased pressure in the eye (secondary angle closure glaucoma).
These eye problems can lead to permanent loss of vision if not treated.
You should call your healthcare provider right away if you have any new eye symptoms, including any new problems with your vision.
Topiramate may cause decreased sweating and increased body temperature (fever). People, especially children, should be watched for signs of decreased sweating and fever, especially in hot temperatures. Some people may need to be hospitalized for this condition. If a high fever, a fever that does not go away, or decreased sweating develops, call your healthcare provider right away.
Topiramate can increase the level of acid in your blood (metabolic acidosis). If left untreated, metabolic acidosis can cause brittle or soft bones (osteoporosis, osteomalacia, osteopenia), kidney stones, can slow the rate of growth in children, and may possibly harm your baby if you are pregnant. Metabolic acidosis can happen with or without symptoms. Sometimes people with metabolic acidosis will:
Feel tired
Not feel hungry (loss of appetite)
Feel changes in heartbeat
Have trouble thinking clearly
Your healthcare provider should do a blood test to measure the level of acid in your blood before and during your treatment with Topiramate. If you are pregnant, you should talk to your healthcare provider about whether you have metabolic acidosis.
Like other antiepileptic drugs, Topiramate may cause suicidal thoughts or actions in a very small number of people, about 1 in 500. Call a healthcare provider right away if you have any of these symptoms, especially if they are new, worse, or worry you:
Thoughts about suicide or dying
Attempts to commit suicide
New or worse depression
New or worse anxiety
Panic attacks
An extreme increase in activity and talking (mania)
Feeling agitated or restless
Trouble sleeping (insomnia)
New or worse irritability
Acting aggressive, being angry or violent
Acting on dangerous impulses
Other unusual changes in behavior or mood
Topiramate may lower bone mineral density. TOPIRAMATE may decrease the density of bones when used over a long period.
Topiramate may have negative effects on growth in children TOPIRAMATE may slow height increases and weight gain in children and adolescents when used over a long period.
Do not stop Topiramate without first talking to a healthcare provider.
Stopping Topiramate suddenly can cause serious problems.
Suicidal thoughts or actions can be caused by things other than medicines. If you have suicidal thoughts or actions, your healthcare provider may check for other causes.
If you have epilepsy and you stop taking Topiramate suddenly, you may have seizures that do not stop. Your healthcare provider will tell you how to stop taking Topiramate slowly.
If you miss a single dose of Topiramate, take it as soon as you can. However, if you are within 6 hours of taking your next scheduled dose, wait until then to take your usual dose of Topiramate and skip the missed dose. Do not double your dose. If you have missed more than one dose, you should call your healthcare provider for advice.
How can I watch for early symptoms of suicidal thoughts and actions?
Pay attention to any changes, especially sudden changes, in mood, behaviors, thoughts, or feelings.
Keep all follow-up visits with your healthcare provider as scheduled.
Call your healthcare provider between visits as needed, especially if you are worried about symptoms.
Topiramate can harm your unborn baby.
If you take Topiramate during pregnancy, your baby has a higher risk for birth defects called cleft lip and cleft palate. These defects can begin early in pregnancy, even before you know you are pregnant.
Cleft lip and cleft palate may happen even in children born to women who are not taking any medicines and do not have other risk factors.
There may be other medicines to treat your condition that have a lower chance of birth defects.
All women of childbearing age should talk to their healthcare providers about using other possible treatments instead of Topiramate. If the decision is made to use Topiramate, you should use effective birth control (contraception) unless you are planning to become pregnant. You should talk to your doctor about the best kind of birth control to use while you are taking Topiramate.
Tell your healthcare provider right away if you become pregnant while taking Topiramate. You and your healthcare provider should decide if you will continue to take Topiramate while you are pregnant.
If you take Topiramate during pregnancy, your baby may be smaller than expected at birth. The long-term effects of this are not known. Talk to your healthcare provider if you have questions about this risk during pregnancy.
Metabolic acidosis may have harmful effects on your baby. Talk to your healthcare provider if Topiramate has caused metabolic acidosis during your pregnancy.
Pregnancy Registry: If you become pregnant while taking Topiramate, talk to your healthcare provider about registering with the North American Antiepileptic Drug Pregnancy Registry. You can enroll in this registry by calling 1-888-233-2334. The purpose of this registry is to collect information about the safety of Topiramate and other antiepileptic drugs during pregnancy.
Before taking Topiramate, tell your healthcare provider about all of your medical conditions, including if you:
Have or have had depression, mood problems, or suicidal thoughts or behavior
Have kidney problems, have kidney stones, or are getting kidney dialysis
Have a history of metabolic acidosis (too much acid in the blood)
Have liver problems
Have weak, brittle, or soft bones (osteomalacia, osteoporosis, osteopenia, or decreased bone density)
Have lung or breathing problems
Have eye problems, especially glaucoma
Have diarrhea
Have a growth problem
Are on a diet high in fat and low in carbohydrates, which is called a ketogenic diet
Are having surgery
Are pregnant or plan to become pregnant
Are breastfeeding or plan to breastfeed? Topiramate passes into breast milk. Breastfed babies may be sleepy or have diarrhea. It is not known if the Topiramate that passes into breast milk can cause serious harm to your baby. Talk to your healthcare provider about the best way to feed your baby if you take Topiramate.
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. Topiramate and other medicines may affect each other causing side effects. Especially tell your healthcare provider if you take:
Valproic acid (such as Depakene® or Depakote®).
Any medicines that impair or decrease your thinking, concentration, or muscle coordination.
Birth control that contains hormones (such as pills, implants, patches or injections). Topiramate may make your birth control less effective. Tell your healthcare provider if your menstrual bleeding changes while you are using birth control and Topiramate.
Ask your healthcare provider if you are not sure if your medicine is listed above. Know the medicines you take. Keep a list of them to show your healthcare provider and pharmacist each time you get a new medicine. Do not start a new medicine without talking with your healthcare provider.
What are the possible side effects of Topiramate?
Topiramate may cause serious side effects including:
See “What is the most important information I should know about Topiramate?”
High blood ammonia levels. High ammonia in the blood can affect your mental activities, slow your alertness, make you feel tired, or cause vomiting. This has happened when Topiramate is taken with a medicine called valproic acid (Depakene® or Depakote®).
Effects on thinking and alertness. Topiramate may affect how you think and cause confusion, problems with concentration, attention, memory, or speech. TOPIRAMATE may cause depression or mood problems, tiredness, and sleepiness.
Dizziness or loss of muscle coordination.
Serious skin reactions. Topiramate may cause a severe rash with blisters and peeling skin, especially around the mouth, nose, eyes, and genitals (Stevens-Johnson syndrome). Topiramate may also cause a rash with blisters and peeling skin over much of the body that may cause death (toxic epidermal necrolysis). Call your healthcare provider right away if you develop a skin rash or blisters.
Kidney stones. Drink plenty of fluids when taking Topiramate to decrease your chances of getting kidney stones.
Low body temperature. Taking Topiramate when you are also taking valproic acid can cause a drop in body temperature to less than 95°F, feeling tired, confusion, or coma.
Call your healthcare provider right away if you have any of the symptoms above.
The most common side effects of Topiramate include:
Tingling of the arms and legs (paresthesia)
Not feeling hungry
Nausea
A change in the way foods taste
Diarrhea
Weight loss
Nervousness
Upper respiratory tract infection
Speech problems
Tiredness
Dizziness
Sleepiness/drowsiness
Slow reactions
Difficulty with memory
Pain in the abdomen
Fever
Abnormal vision
Decreased feeling or sensitivity, especially in the skin
You are encouraged to report negative side effects of prescription drugs to the FDA. Visit www.fda.gov/medwatch or call 1-800-FDA-1088.
The above health information is provided for educational purposes only and is not intended to replace discussions with a healthcare provider. All decisions regarding patient care must be made with a healthcare provider, considering the unique characteristics of the patient. The product information provided is intended only for residents of the United States. The products discussed herein may have different product labeling in different countries.
Every patient begins care with a comprehensive medical evaluation. This step helps determine whether medical care is appropriate and safe, and to understand what may be contributing to changes in weight, metabolism, or overall health.
The clinical review may include assessment of medical history, current medications, weight and health patterns, relevant risk factors, and other information needed to understand the broader clinical picture before any treatment decisions are made.
Not every patient is eligible for treatment. During review, the physician evaluates medical appropriateness, potential risks, and contraindications. If care is not appropriate, treatment will not be provided.
All decisions are made by a licensed, board-certified physician based on clinical judgment, safety standards, and individual health needs. There are no automated approvals or one-size-fits-all plans.
Lifestyle factors influence metabolic health and long-term wellbeing. Guidance in this area is used to support how the body functions, not to promote rigid programs or universal plans.
Nutritional guidance focuses on supporting metabolic health and sustainability. Recommendations are individualized and may address eating patterns, meal consistency, food quality, and factors that influence blood sugar and energy balance.
Guidance around movement is designed to be realistic and appropriate for each individual. This may include discussion of daily activity, strength, flexibility, and aerobic movement as they relate to metabolic health and function.
Lifestyle guidance is medically informed, integrated into an overall care plan, and adjusted based on physiology. It does not rely on motivation tactics, accountability coaching, or prescriptive programs.
Medications are considered only after medical evaluation and clinical review. Medication is not required for every patient and is never prescribed automatically.
Medication decisions are based on medical history, potential risks and benefits, contraindications, and individual health needs. Not all patients qualify for medication.
When medically appropriate, medications that may be considered include GLP-1 receptor agonists, metformin, and bupropion-containing therapies. These are examples, not guarantees of treatment.
Some medications are FDA-approved brand medications, while others may be compounded formulations prepared by licensed pharmacies. Compounded medications do not undergo FDA approval in the same way as FDA-approved brand medications. The choice of medication, if any, is determined through physician review.
Some medications are FDA-approved brand medications, while others may be compounded formulations prepared by licensed pharmacies. Compounded medications do not undergo FDA approval in the same way as FDA-approved brand medications. The choice of medication, if any, is determined through physician review.
Medication management is physician-directed and safety-focused. It is not a medication menu, a guarantee of access, or a substitute for medical judgment.